| Topic | Burns |
| Author | Henry Murphy |
| Duration | Up to 2.5 hrs with options for further advanced discussion |
| Equipment required | Projector, computer, and internet connection for demonstration of diagrams and resources |
● Basics (15 mins)
● Main session: (2 x 20 minute) case discussions covering the key points and evidence
● Optional Advanced session: (3 x 20 minutes) case discussions covering grey areas, diagnostic dilemmas; advanced management and escalation
● Sim scenario (30-60 mins)
● Quiz (10 mins)
● Summary (5 mins) and 5 top tips
Expectation is for the learners to have read some of these links before the session.
Minor burns
Airway burns
LITFL management
Children’s Burns Trust
This is an excellent talk from DFTB18
PEM playbook major burns podcast. (It also has some really nice resources on the notes page)
Good recent review article – “Early management of paediatric burn injuries” by Gill and Falder
The World Health Organisation defines a burn as “… an injury to the skin or other organic tissue primarily caused by heat or due to radiation, radioactivity, electricity, friction or contact with chemicals”.
This is an important definition, as burn injuries are managed distinctly from other injuries such as lacerations. The first aid applied to a burn should usually include running under cool water for 20 minutes- as soon as possible and within 3 hours if able. Burns may cause irreversible coagulation to the skin, but around this is an area of ‘stasis’ where skin damage can be reversed. Cool water as first aid has been shown to reduce the need for plastic surgery with skin grafting by 44.1% (take a look at the review of this evidence by DFTB’s Andy Tagg).
The skin consists of different layers. We can use our knowledge of the anatomy of these layers to grade the damage to the skin from a burn. The specialist organs within the skin can be damaged – assessing the function of these should form part of your history and examination of a burn.
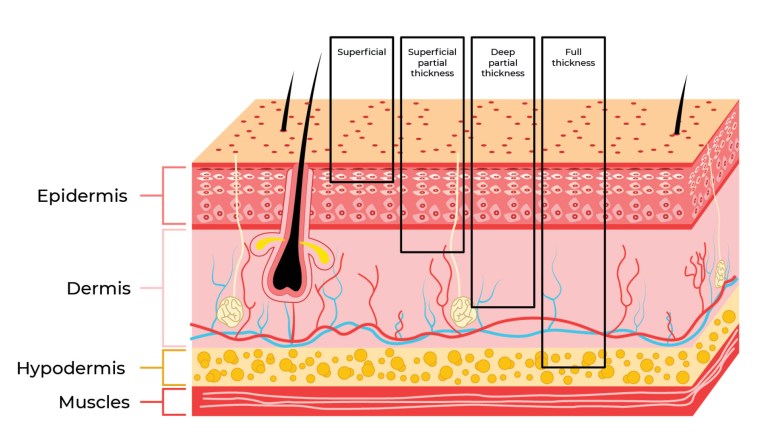
A superficial or epidermal burn affects the epidermis only and may look red and swollen due to a temporary increase in blood flow, but there is no blistering or skin loss. It may be painful because the nerves are not damaged. They usually heal well.
A partial thickness burn involves the epidermis and part of the dermis, and presents as either a blister or as peeling:
In superficial partial thickness burns, the underlying blood vessels and nerves are still intact and so these burns are painful and sensate. The underlying skin will blanch on pressure as the blood vessels are intact in the dermis. A small burn may heal by itself without a scar.
Deep partial thickness (or deep dermal) burns damage most of the dermis and the nerves and blood vessels are variably damaged. The capillary refill may be delayed or absent, and sensation may be variable or absent.
A full thickness burn passes beneath the dermis and can damage the blood vessels, nerves and tissues beyond such as muscle and bone. This may look pale, may not blanch, and may be insensate and painless. The hair follicles may be damaged and this burn will likely need surgery. The skin may lose its pigment when it heals.
This infographic from the London and South East of England Burn Network is a great one stop pictorial resource for grading burns.
Types of Burn
It is important to know what has burned the skin, as the mechanism may dictate the management.
Heat. Cooling first aid is essential. Contact time with the heat source may not be as important as the source itself – a brief contact with a flame may only singe the hair, whereas a hot oil splash in a kitchen will more likely lead to full thickness burns. Think about the burning material – was it likely to give off smoke containing carbon monoxide or even cyanide?
Chemical. Staff and the patient must wear appropriate PPE to protect eyes and unaffected skin. First aid is essential and may require well in excess of 20 minutes. If powder is present on the skin, this should be brushed off before irrigation. If it will not delay first aid, try to check the pH of any area of skin damage before irrigation. Some hospitals have neutralising sprays or other solutions to use for chemical burns such as Diphoterine – start with Hartmans or Normal Saline if you do not have this to hand. Skin damage may continue due to penetration of the chemical into the dermis. Make sure you check the eyes for splash or contact burns too.
Electrical. There may be no visible surface burn, but the current can travel along fascial planes and can cross the body. Look for entry and exit points (may be very small) and consider important structures in between – particularly the heart. An ECG is essential. Check a CK and possibly troponin. Beware of compartment syndrome.

Radiation. Sunburn is a form of radiation burn – if the skin is not lost, the management is painkillers and oral hydration. Larger burns may need specialist input but deep sunburn is unusual and in a child would raise concern regarding safeguarding. Acute ionising radiation burns from an accident or industrial source require early specialist help. Consider the risk to staff from a radiation exposure. Measuring a radiation dose can be done using a Geiger counter. Delayed skin reactions to therapeutic radiation are not classified as burns, but as a form of dermatitis.
Friction burns. These can be a combination of a traumatic injury to the skin and a thermal burn. Apply first aid and ensure care is taken to remove debris. ‘Road rash’ is grit and other material from the ground implanted into the skin during a slide – classic in a fall from a motorbike. If not removed, this can cause infection and can permanently tattoo the skin. Discuss with a plastic surgery or burns team if contaminated, deep, large or over a particularly important area such as the face, genitals or hands. More information on friction burns can also be found in this DFTB article.
Frostbite is skin damage, but is not classified as a ‘burn’.
Non accidental injury
Scald burns are the most common burn type in children who have been abused and the most common causative agent is tap water. Abusive scalds tend to be distributed on the buttocks, perineum, and lower extremities, with clear upper limits and scald symmetry especially when present on the lower extremities. In non-scald abusive burns contact burns are the most common. These burns tend to be distributed on the back, shoulders, and buttocks, with clearly demarcated edges often matching the object used.
The prevalence of abusive burns is estimated to be 5.3% – 14% of children admitted to burns units 1-3 highest for those aged 0 – 1 years.
Hodgeman, Pastorek, Saeman et al (2016) found that children with abusive burns were significantly younger than those with accidental burns. However when compared to children referred to child protection teams for all causes of physical abuse, those with burns were significantly older and more likely to be boys (66% vs. 56%).
This RCPCH review of child protection evidence in burns is a must read.
A 15 year old girl was cooking in the kitchen an hour ago and accidentally spilled a pan of hot water from the hob onto her hip whilst wearing jeans. With assistance from her mother, she immediately ran the burn under cold water for 20 minutes in the shower. They have attended the Emergency Department as the burn has begun to blister.

How would you manage the blistered areas of this burn?
What analgesia would you use?
How would you size this burn?
What advice would you give about risks during the first few days after the burn?
Sizing and grading a blistered burn
This skin is blistered. How to manage a blister is a controversial topic. Some clinicians say that grading and sizing a burn cannot occur without an assessment of the underlying skin surface. These clinicians would advocate for removing the devitalised tissue, known as debridement or ‘deroofing’. Those against deroofing believe that the intact skin and fluid within a blister protect the healing skin, acting as a natural dressing. We would recommend you follow your local guidelines in this area.
This is the same burn being deroofed, and after being deroofed.

As you can see, it looks quite different, and the skin surface can now be assessed for the burn depth. This wound is a better representation of the actual tissue damage.
Accurate assessment can help make the decision for appropriate early referral for skin grafting.
More on deroofing with a ‘how-to’ guide from the British Burn Association here.
Analgesia
Proper deroofing or debridement of a burn can be very painful.
If a competent member of your hospital team can deroof this blister, this can occur locally.
A deep burn may actually be insensate. Give simple analgesia plus an opiate (orally, intranasally or intravenously) and make an initial assessment.
This DFTB page looks into pain assessment and analgesia.
If painful, consider procedural sedation, for example, ketamine or nitrous oxide -involve senior staff in the paediatric emergency department or anaesthetic service.
This procedure may even need to be done in theatre, but if this is required, it usually would involve a transfer to your local Burns Service.
Burn sizing
The Lund and Browder chart should be used as seen below. The front and back of the patient make up 50% of the total body surface area (easy to forget!) The chart allows for partial and full thickness to be graded separately.

The Mersey Burns app allows you to size a burn very easily. You can enter the age and weight of the child, which will automatically calculate the percentage body surface area for the burn you have entered.

An alternative is the New South Wales trauma app:
Risks during the initial post-burn period
(From Leicester Children’s Hospital)
Toxic Shock Syndrome (TSS) is an acute, multi-system inflammatory response to an exotoxin-mediated bacterial infection. It is a rare but life-threatening condition, with rapid progression to septic shock and multi-organ failure. The most common risk factor for TSS in the UK is a small surface area burn in a child. It is typically associated with children aged 1-4 years, two days after a small burn.
TSS must be suspected in a child with a recent history of a burn or other risk factors, who is systemically unwell, with or without a rash.
These Center for Disease Control criteria can help diagnose TSS:

Read more about diagnosing and managing TSS here.
A 3 year old girl was standing close to a petrol-soaked barbeque as her brother lit the coals. Her clothing caught fire and her family put out the flames, but her clothing was not removed, and no first aid cooling was performed. The family called for an ambulance, and you are now called to assess the burn in the Emergency Department 1.5 hours after the injury.

How would you assess this injury?
Is this a burn that needs fluid resuscitation?
Where would you refer the burn? Does this burn need referral?
Initial Assessment of a Large Burn
Burns are a traumatic injury, and the energy of the heat source itself (such as an explosion or electrical burn) or the act of self-extrication may have caused secondary injury. Put out a priority call to your hospital switchboard – some hospitals would put out a ‘trauma’ call for burns, whereas others have a dedicated ‘Burns’ priority call.
Take an ABCDE approach. A summary from Vicburns is provided below – as you can see, the assessment is extensive. Consider asking the most experienced team member to lead the assessment – this may be you or another Paediatric colleague, but do ask your colleagues in Emergency Medicine, Surgery and Orthopaedics for help- they may have seen previous injuries or have rotated through a Burns service before.

Fluid management
After the Primary Survey, the size of the burnt areas can be recorded. Remember that erythema only without blistering or skin loss is not counted as a burn for the purposes of burnt body surface area.
A burn of greater than 10% in children requires intravenous fluid management. The Parkland formula can be used to calculate this (other formulae are also available. It is suggested that you use your local guidance).
4ml x TBSA (%) x body weight (kg); 50% given in first eight hours; 50% given in next 16 hours.
The Parkland formula can be found on MDcalc.
The Mersey Burns app can also automatically calculate the Parkland formula for you.
There is discussion over the volume of fluid resuscitation to use within the Parkland formula for Paediatric patients, with some centres now using 3ml/kg rather than 4ml, for example this service in New South Wales, Australia. Be aware that formulas usually calculate additional fluid resuscitation for the burn only. Usual maintenance hydration should continue alongside this.
Referring a burn
The Burn Networks
Burn Services are similar to trauma care – every hospital Emergency Department will care for burned patients, but severe surgical cases will need discussion or referral to a specialist tertiary service.
In the UK burns services are divided into Networks, as seen below.

Specialist care is delivered at Burn Centres, Units and Facilities:
Burn Centres – This level of in-patient burn care is for the highest level of injury complexity and offers a separately staffed, geographically discrete ward. The service is skilled to the highest level of critical care and has immediate operating theatre access.
Burn Units – This level of in-patient care is for the moderate level of injury complexity and offers a separately staffed, discrete ward.
Burn Facilities – This level of in-patient care equates to a standard plastic surgical ward for the care of non-complex burn injuries.
The suggested minimum threshold for referral into specialised UK burn care services can be summarised as:

Australasian Burns are organised by territory in Australia, or nationally in New Zealand. This website contains all burns services and their contact details.
Referral criteria are as follows:
● Burns greater than 10% Total Body Surface Area (TBSA)
● Burns greater than 5% TBSA in children
● Full Thickness burns greater than 5% TBSA
● Burns of Special Areas – Face, Hands, Feet, Genitalia, Perineum, Major Joints and circumferential limb or chest burns
● Burns with inhalation injury
● Electrical burns
● Chemical burns
● Burns with pre-existing illness
● Burns associated with major trauma
● Burns at the extremes of age – young children and the elderly.
● Burn injury in pregnant women
● Non-accidental burns
30 minutes ago, 8-year-old Billy fell from a first-floor window, trying to escape a house fire. Paramedics were on scene within 10 minutes. They parcelled him up and put him in the back of the ambulance. His oxygen saturations were 95% in air, respiratory rate 30, heart rate 150 and systolic BP 100. They gave him high flow oxygen via a non-rebreathe mask. He was in a lot of pain, so they covered his burns with cling film, gave some morphine and set off for your Emergency Department.
You lead the burns team and your SHO tells you that on their primary survey, they note a contusion over the child’s chest and abdomen. Billy remains tachycardic despite fluid resuscitation and analgesia.
How would you proceed?
How not to be burned by burns
This case is from How not to be burned by burns Part 2: Major burns and discusses the likelihood of traumatic associated injuries.
Discussions should centre around a thorough A-E assessment to ensure a traumatic injury secondary to blast or blunt trauma is not missed. Trauma imaging protocols should be used such as should Royal College of Anaesthetist Paediatric Trauma Protocols.
This CATS burns management document discusses the approach to the burn in a similar way to trauma patients. A burn is a complex injury, but we must always consider additional traumatic forces may have been sustained due to self extrication or the burning environment, such as falling masonry.
This fantastically thorough Blast Injury Manual walks you comprehensively through the journey of the patient and staff, from actions at the prehospital site of an explosion, through to ethics and team care.
So you’re on shift in Paeds ED on Thursday evening at 6pm, you’re due to finish at 7pm and just starting to think about that glass of wine, the sofa and the next episode of your current Netflix box set.
The sister from resus comes through to let you know about an imminent blue call of a 13 year old girl involved in a chemical attack with suspected acid burns to her face and eyes and upper chest arriving in 10 minutes.
How would you prepare the team?
What can you do to manage the burn?
How would you prepare the team & what can you do to manage the burn?
This DFTB post on chemical burns is great for a next level discussion about pH, Diphoterine, and safeguarding.
A 4 year old girl presents with right hand burns after inserting a kitchen knife into an electrical socket at home.
How would you manage this case differently compared to a simple thermal burn?
.
How would you manage this case differently compared to a simple thermal burn?
This PEM Playbook has a great set of questions to ask in the history specific to electrical exposure.
See the simulation from EM3 here.
A 1 year old boy is brought to Paediatric ED by his father at 0100 on a Saturday nightshift. He reports the bath run at 7pm was too warm and after going to bed his son was unsettled. He weighs 9.5kg.

Question 1
You see evidence of skin loss over the front and back of the arm at the level seen here. How would you size this burn?
A: 4.5%
B: 9%
C: 18%
D: 40%
Answer 1
Answer A
This burn involves the hand and half the forearm. According to the Lund and Browder chart, the front and back of the forearm and hand each constitute 1.5% of the total body surface area.
Both sides of the hand = 3%. 1/2 the forearm is 1.5% = 4.5 roughly. Therefore the closest answer is 4.5%.
Question 2
Does this child require fluid management? If so, how much?
A: Oral fluid challenge 5ml every 5min
B: 20ml/kg bolus (so 300ml) and assess response
C: No fluid resuscitation needed
D: 3 or 4ml x burn surface area (%) x kg. 50% given in first eight hours; 50% given in next 16 hours
Answer 2
Answer C
As this burn is less than 10% of total body surface area, specific fluid management is not required.
Question 3
Where would you refer this child for management of the burn?
A: Paediatric team on call
B: Burns Service
C: General Surgical Theatres for urgent debridement
Answer 3
Answer B
This burn is significant – it involves the hand and is also over 2% of the total body surface area and therefore should be referred to a specialist Burns service.
Question 4
Who else would you involve in the management of this case?
A: Paediatric safeguarding team
B: Paediatric and/ or ED Consultant
C: Clinical Photography
Answer 4
Answer D
This burn appears linear, which may indicate forced immersion in hot water. The history suggests a delay in presentation which also raises suspicion of a non-accidental burn. A safeguarding referral should be made.
The most senior doctor within the Department should be made aware of the case. Accurate photographic documentation of the burn at presentation would be vital for any subsequent investigation.



