The Choosing Wisely® campaign is an initiative that promotes collaborative conversations between clinicians and families to safely avoid unnecessary and potentially harmful tests.
The American Academy of Paediatrics Section on Emergency Medicine (AAP SOEM) created a list of five key recommendations for Paediatric Emergency Medicine after a structured review process and expert consensus opinion.
This series of DFTB articles aims to increase awareness of the Choosing Wisely® recommendations. Each article will take a deeper dive into each recommendation’s supporting evidence and practical implications.
Do not order laboratory testing or a CT scan of the head for a patient with an unprovoked, generalized seizure or a simple febrile seizure who has returned to baseline mental status.
The parents of 18-month-old Susie brought her to the Emergency Department after she had a seizure at home.
She has had two days of coryzal symptoms and fever. Following the seizure, and a post-ictal period, she has returned to her baseline and is playful with no focal neurologic symptoms or concerning examination features.
Her parents ask you whether any blood tests or brain scans are needed
What do the guidelines say?

Seizures in children can be caused by a wide group of conditions, ranging from benign or idiopathic causes to genetic, intracranial, or systemic abnormalities. Many organisations have published guidance, such as NICE, SIGN, AAP, and the Paediatric Improvement Collaborative, whilst the International Alliance Against Epilepsy website includes further international and regional guidance.
In the case of simple febrile seizures or typical unprovoked generalised seizures, when the child has returned to baseline, guidelines recommend against performing laboratory measurements such as electrolytes, glucose, or inflammatory markers.
The history and examination findings should guide any laboratory investigations of a provoked generalised or complex febrile seizure. Similarly, CT imaging is not recommended for febrile seizures or typical unprovoked generalised seizures when the child fully recovers.
If indicated, MRI is the investigation of choice, and although this should take place as soon as possible, it may be appropriate for this to occur as an outpatient. The American College of Radiology guidelines provide further detail on imaging recommendations based on different age and seizure type variants.
What is the evidence for avoiding laboratory testing?
Evidence for the usefulness of laboratory testing is limited, with recommendations based on small to medium-sized observation studies and expert consensus opinion.
One single-centre retrospective cross-sectional study involving 549 children with simple febrile seizures evaluated potential laboratory abnormalities. Investigators found that 99.3% of blood glucose levels, 98% of calcium, and 99% of electrolytes and renal function tests were normal. The proportion of children with abnormal findings on investigations was exceptionally low and of no clinical significance.
What is the evidence for avoiding imaging?
In epilepsy that is not typically associated with structural brain abnormalities (such as febrile seizures or idiopathic generalised epilepsy), there is a limited role for CT imaging, particularly in the acute setting. Despite international and regional guidelines discouraging its use, many children with generalized seizures still get a CT.
An expert committee appraised the evidence behind recommendations to avoid imaging to inform the 2022 NICE guidance. The literature search generally identified low to very low-quality observational studies looking at the general use of CT for children who have had a seizure to identify scarring abnormalities, inflammatory/infective/immune abnormalities, and tumours. From 18 observational studies involving 1803 children, 3% (95% CI 2 – 4%) had scarring abnormalities on CT. For inflammatory/infective/immune abnormalities, 19 observational studies involving 308 children found 15% (95% CI 7 – 28%) to have abnormalities on CT. When considering tumours, 37 observation studies involving 2661 children found that 3% (95% CI 1-7%) had tumours. It is important to note that the combined results from these studies did not narrow these down to children who had returned to baseline. Despite this, the results highlight the importance of how a careful history and examination can limit the use of CT.
Although acute imaging has a limited role for simple febrile seizures and generalised seizures with a return to baseline, the opposite is true for patients with focal seizures. Imaging abnormalities are considerably higher in children with focal seizures or focal neurologic signs, with up to 50% having abnormalities detected on CT. When indicated, imaging should be performed only after the child is stabilized and seizures have stopped.
MRI is the study of choice when imaging is recommended due to its superior anatomic resolution, pathology identification, and lack of radiation risk. However, it is important to note that sedation for the scan may also confer risk in the emergent setting.
Which children need laboratory testing and imaging?
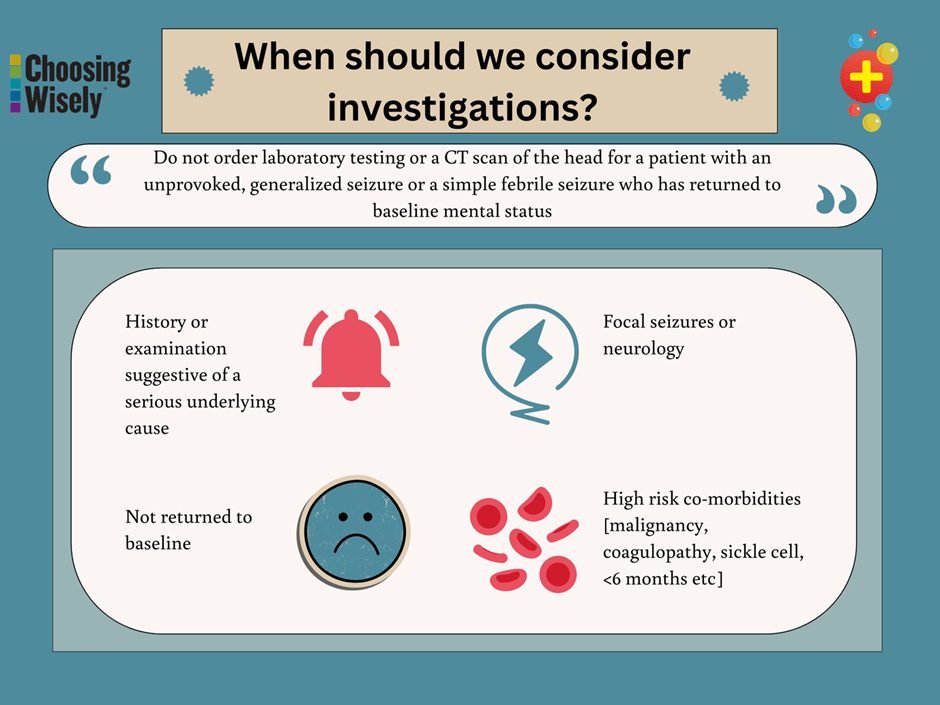
Laboratory tests should be ordered based on the individual clinical manifestations of the child. This may include specific clinical findings such as evidence of diarrhoea or vomiting, dehydration, meningitic signs, a history of significant head trauma immediately preceding the seizure, or failure to return to baseline.
A CT scan may also be indicated in children who have not returned to baseline and those with a focal seizure, focal neurology, or high-risk co-morbidities (such as malignancy, coagulopathy, sickle cell disease, or age < 6 months).
What should we say to parents and caregivers?
Seizures are frightening for parents and caregivers, who can often fear the worst. It is important to recognise and acknowledge their concerns. An explanation of the diagnosis and why seizures occur can be useful.
Parents and caregivers should be reassured that since their child has returned to normal, further investigations are unlikely to identify anything that a careful history or examination would not pick up.
Investigations are unlikely to change management but can cause unnecessary distress for their child, whilst unnecessary radiation may increase the risk of future malignancy. Discussion may be supported by patient information materials, particularly the provision of information in multiple languages. Epilepsy charities can also be a useful source of information and support for parents and caregivers.
Take home points

Take a look at…
References
American Academy of Pediatrics, Subcommittee on Febrile Seizures. Neurodiagnostic evaluation of the children with a simple febrile seizure. Pediatrics. 2011;127(2):389-394. DOI: https://doi.org/10.1542/peds.2010-3318
Brugman J, Solomons RS, Lombard C, Redfern A, Du Plessis AM. Risk-Stratification of Children Presenting to Ambulatory Paediatrics with First-Onset Seizures: Should We Order an Urgent CT Brain?. J Trop Pediatr. 2020;66(3):299-314. doi:10.1093/tropej/fmz071
Expert Panel on Pediatric Imaging, Trofimova A, Milla SS, et al. ACR Appropriateness Criteria® Seizures-Child. J Am Coll Radiol. 2021;18(5S):S199-S211. doi:10.1016/j.jacr.2021.02.020
Fine A, Wirrell EC. Seizures in Children. Pediatr Rev. 2020;41(7):321-347. doi:10.1542/pir.2019-0134
Hirtz D, Ashwal S, Berg A, et al. Practice parameter: Evaluating a first nonfebrile seizure in children. Report of the Quality Standards Subcommittee of the American Academy of Neurology, the Child Neurology Society, and the American Epilepsy Society. Neurology. 2000; 55(5):616-623. Reaffirmed October 17, 2020
Jaffe M, Bar-Joseph G, Tirosh E. Fever and convulsions: indications for laboratory investigations. Pediatrics. 1981;67(5):729 –731
Maytal J, Krauss JM, Novak G, Nagelberg J, Patel M. The role of brain computed tomography in evaluating children with new onset of seizures in the emergency department. Epilepsia. 2000;41(8):950-954. doi:10.1111/j.1528-1157.2000.tb00277.x
McKenzie KC, Hahn CD, Friedman JN; Canadian Paediatric Society, Acute Care Committee. Emergency management of the paediatric patient with convulsive status epilepticus. Paediatr Child Health. 2021;26(1):50-57
NICE. Epilepsies in children, young people and adults; Evidence reviews underpinning recommendations. NICE guideline NG217. 2022. Accessed online at https://www.nice.org.uk/guidance/ng217/evidence/b-computed-tomography-scan-performance-in-people-with-epilepsy-pdf-398366282811
NICE. Epilepsies in children, young people and adults. NICE guideline NG217. 2022. Accessed online at https://www.nice.org.uk/guidance/ng217
Reinus WR, Wippold FJ, 2nd, Erickson KK. Seizure patient selection for emergency computed tomography. Ann Emerg Med 1993;22:1298-303.
Riviello JJ Jr, Ashwal S, Hirtz D, et al; American Academy of Neurology Subcommittee; Practice Committee of the Child Neurology Society. Practice parameter: Diagnostic assessment of the child with status epilepticus (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2006;67(9):1542-1550
Royal Children’s Hospital Melbourne. Afebrile Seizures. 2020. Accessed online at https://www.rch.org.au/clinicalguide/guideline_index/afebrile_seizures/
Sawires R, Buttery J, Fahey M. A Review of Febrile Seizures: Recent Advances in Understanding of Febrile Seizure Pathophysiology and Commonly Implicated Viral Triggers. Front Pediatr. 2022;9:801321. Published 2022 Jan 13. doi:10.3389/fped.2021.801321
Subcommittee on Febrile Seizures; American Academy of Pediatrics. Neurodiagnostic evaluation of the child with a simple febrile seizure. Pediatrics. 2011;127(2):389-394. doi:10.1542/peds.2010-3318
Veerapandiyan A, Aravindhan A, Takahashi JH, Segal D, Pecor K, Ming X. Use of Head Computed Tomography (CT) in the Pediatric Emergency Department in Evaluation of Children With New-Onset Afebrile Seizure. J Child Neurol. 2018;33(11):708-712. doi:10.1177/0883073818786086
Young AC, Costanzi JB, Mohr PD, Forbes WS. Is routine computerised axial tomography in epilepsy worth while?. Lancet. 1982;2(8313):1446-1447. doi:10.1016/s0140-6736(82)91340-x
Yousefichaijan P, Dorreh F, Abbasian L, Pakniyat AG. Assessing the prevalence distribution of abnormal laboratory tests in patients with simple febrile seizure. J Pediatr Neurosci. 2015;10(2):93-97. doi:10.4103/1817-1745.159180














