3-year-old Thomas has been eating soil. He looks pale, and his bloods show a microcytic hypochromic anaemic with Hb 80g/dL and low MCV. It looks like he has iron deficiency anaemia.
Now what?
Anaemia is insufficient red blood cells or haemoglobin (Hb) and affects 33% of the world’s population. Half of these cases are due to iron deficiency. Around 42% of children under five are anaemic. As haemoglobin reference values are age and sex-specific, it is important to use appropriate ranges from the laboratory that performed the testing when interpreting results.
Iron deficiency is the commonest cause of anaemia in children
When taking a history, ask about the ethnic background of the child. Certain ethnic groups are more prone to having a specific haematological condition, such as thalassaemia – more common in in Mediterranean and Southeast Asians.
Take a dietary history, and ask specifically about breast and cow’s milk intake, as well as iron intake. Iron-rich foods include red meat, spinach and tofu. Milk is a poor source of iron and fills children up, reducing their appetite and desire for other food. Children over 12 months of age should drink less than 500-750mL of cow’s milk a day.
G6PD deficiency is also a potential cause of anaemia (through haemolysis), so ask about specific triggers such as broad bean ingestion, medications (e.g. co-trimoxazole, sulphonamides) as well as symptoms of haemolysis (i.e. dark-coloured urine, jaundice, scleral icterus). There may also be a family history of anaemia, jaundice, gallstones or splenomegaly.
Key things to explore:
- Infants and toddlers (up to 36 months): maternal iron deficiency, prematurity/low birth weight, low intake of iron-rich food, excessive cow’s milk consumption
- Children and adolescents: a vegetarian or vegan diet, gastrointestinal disorders (e.g. coeliac disease), heavy menstrual bleeding
Children and adolescents with low iron usually present with impaired cognitive function. They may have poor memory and concentration, behavioural disturbances and restlessness or lethargy. They may also display pallor, poor growth, weakness or shortness of breath. Occasionally they have pica. When children have pica, they eat things that are not considered food. This includes soil, paper and wood.
Thomas looks lethargic and pale. He does not appear jaundiced, so you suspect his anaemia is not due to haemolysis, but you make sure the lab runs a bilirubin on his biochemistry sample.
In all forms of anaemia, the heart compensates by pumping faster to deliver more oxygen to the vital organs. Longstanding anaemia can result in prolonged cardiac stress, resulting in arrhythmias, a flow murmur and high-output cardiac failure.
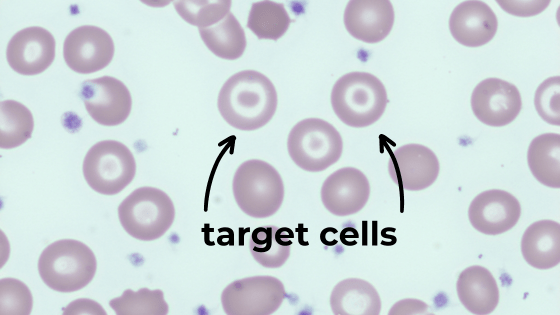
You ask the laboratory to run a blood film. It shows target cells and pencil cells.

Laboratory tests
Important blood tests in suspected cases of anaemia include:
- Full blood count – in iron deficiency anaemia, the red blood cells will be microcytic (low MCV) and hypochromic (low MCHC)
- Blood film – you may see target cells or pencil cells
- Iron studies – ferritin is key to diagnosis
- Reticulocyte count to look at bone marrow’s response to the anaemia – a high reticulocyte count means increased response to blood loss/haemolysis, whereas low or normal reticulocyte count means a reduced response to the anaemia.
- Bilirubin – to look for haemolysis
The easiest way to think of differentials is to classify the anaemia based on the cell size (MCV):
Microcytic anaemia (low MCV)
Consider: iron deficiency, thalassaemia
When faced with a low MCV, consider doing iron studies and/or haemoglobin studies.
Serum ferritin <20μg/L suggests borderline or low iron stores.
Ferritin is an acute phase reactant. This means that a normal result does not mean the child does not have an iron deficiency if there is a coexisting infection or inflammatory process. NB: Serum iron levels reflect recent iron intake.
Normocytic anaemia (normal MCV)
Consider: haemolysis, blood loss, marrow hypoplasia, leukaemic infiltration
When the MCV is normal, consider a reticulocyte count, LDH, DAT (Coombs test), haptoglobin, G6PD assay, and hereditary spherocytosis screen. If the reticulocyte count is low, this raises concerns about the bone marrow’s response.
Macrocytic anaemia (high MCV)
Consider: B12 deficiency or folate
Oral iron therapy is the first-line treatment
Treatment should be started when the child’s serum ferritin is low (<20μg/L).
Modify their diet and increase intake of iron-rich food, reduce cow’s milk input and consider making a referral to a dietitian.
Then, start treatment with 3mg/kg/day of elemental iron. They need to take this for a minimum of three months. They should have a repeat full blood count and ferritin after three months to assess progress. Taking iron supplements with ascorbic acid (vitamin C) in the form of orange juice helps absorption.
Iron supplements often cause constipation, black stools, abdominal discomfort, and may stain teeth. Most of these symptoms will settle within a week of starting the medication. Alternatively, 6mg/kg on alternate days may be better absorbed with fewer side effects. There are lots of different preparations, so it is important to note the concentration of elemental iron provided.
Intravenous iron infusions are rarely required in children. Blood transfusions should only be considered for patients who are actively bleeding or haemodynamically unstable.
Thomas has a low serum ferritin level.
He is referred to a dietician, who helps his parents reduce his milk intake.
He’s started on oral iron, and a repeat full blood count after three months shows a significant improvement in his haemoglobin.
References
- https://www.rch.org.au/clinicalguide/guideline_index/Anaemia/
- https://www.rch.org.au/clinicalguide/guideline_index/Iron_deficiency/
- https://pch.health.wa.gov.au/For-health-professionals/Referrals-to-PCH/Prereferral-guidelines/Iron-deficiency-and-iron-deficiency-anaemia
- https://raisingchildren.net.au/guides/a-z-health-reference/anaemia
- https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(20)32594-0.pdf
- https://www.who.int/health-topics/anaemia#tab=tab_1
- https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/iron-deficiency#iron-deficiency














